The holy grail for the management for peri-implantitis is bone regeneration and re-osteointegration. These are difficult to achieve reliably and in fact most histological studies indicate that true reintegration is unpredictable and difficult to achieve. From a practical clinical perspective, we aim to achieve a pocket depth reduction to manageable levels (ie less than or equal to 5mm), no bleeding on probing and no erythema or suppuration around an implant. The German group lead by Frank Schwartz published a key study ( Schwartz et al 2009) demonstrating the clinical success of use of particulate bovine bone graft materials and barrier membranes in the management of intrabony defects around implants. Further analysis of their patient subsets demonstrated (Schwartz et al 2010) the impact of the defect anatomy (1,2,3 walls) on the regenerative potential around an implant. One aspect that was overlooked in this article is the overall alveolar anatomy and the thickness and orientation of the buccal bone on the surrounding teeth and implants. This has a strong influence on the regenerative potential and the clinical outcome.
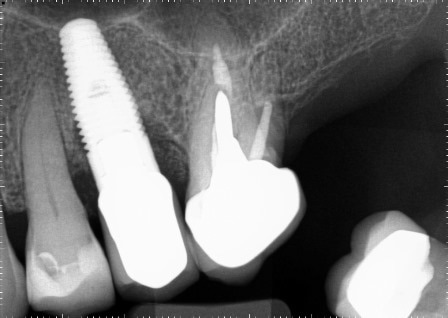
This case demonstrates the effect of the ridge morphology on the extent of regeneration. The UL5 implant was an immediate implant placed 5 years prior to the patients referral to my care at Bowlane Dental. The patient was flagged up as a high risk patient by her dental hygienist due to the suppuration and edema affecting the soft tissues around the implant. As a result of the 9mm buccal pocket, the patient was diagnosed with an advanced peri-implantitis lesion despite the deceptive radiographic appearances. Surgical assessment and treatment were indicated rather than non surgical debridement which has been demonstrated as ineffective in the severe cases. Surgical exploration revealed a 2 walled defect interproximally and advanced bone loss on the buccal aspect despite an attempt at GBR during implant placement and also at the time of exposure.
We elected to attempt bone regeneration around UL5 due to the thickness of the buccal bone on the neighboring teeth. This was undertaken with particulate bovine graft materials as well as a de-epithelialised free gingival graft as a substitute for Collagen barrier membrane due to it ability to facilitate closure and an improvement of soft tissue thickness.
The regenerative surgery was followed by month supportive post-surgical maintenance by the hygienist team which consisted of plaque control advice and supragingival debridement of the implant and surrounding teeth. Six month reassessment reveal a healthier clinical situation with a 4mm buccal probing depth, resolution of erythema and suppuration and no bleeding. We also noted residual 2mm of recession which could be easily corrected but the patient was happy with the result given her low lip line. I would like to thank Sarah Urquhart for referring this patient in a timely manner and also for the diligent supportive therapy without which it would have been difficult to achieve this excellent result.